Higashi says monkeypox not a great threat to students, but polio can strike anyone unvaccinated
REQUIRED: Dr. Higashi said it would be difficult for a Shalhevet student to get an exemption from the polio vaccine.
November 28, 2022
Members of the Shalhevet community are at low-risk for contracting monkeypox, according to infectious disease expert Dr. Julie Higashi, while polio is a more serious challenge – though only for the unvaccinated.
Monkeypox cases started appearing in May, with the World Health Organization saying that cases had “mainly but not exclusively been identified amongst men who have sex with men,” a group now WHO and other health groups now abbreviate as “MSM.”
Dr. Higashi, who previously served on Shalhevet’s Medical Task Force and is the mother of junior Tomomi Shaw, said that individuals not in that population are at a much lower risk of catching monkeypox. She added that cases when children have caught monkeypox have been when someone in their households had the virus.
But she said anyone unvaccinated who was exposed to polio would be at risk for contracting the illness.
Polio, which can be asymptomatic and contagious but also can cause paralysis and death, has been found in wastewater in Rockland and Orange counties, New York. According to media reports, polio also has been found now in wastewater in New York City and parts of Long Island, a large New York suburb.
An “unvaccinated immunocompetent young adult” – who is Orthodox Jewish, according to media reports – was diagnosed in Rockland County in June with a case of paralytic polio, meaning that this individual now has paralysis. There is no cure for polio-induced paralysis.
In Rockland County, as of Aug. 1 only about 60% of individuals were vaccinated for polio according to the New York State Department of Health, and in some zip codes in the county vaccination rates for polio were as low as 37.3%.
“So as long as there are pockets of people who are unvaccinated and they overlap with a population that might be circulating polio, there is a risk for us to have cases of [paralytic] polio in LA County,” Dr. Higashi said in an interview.
Dr. Higashi said the polio circulating now is a vaccine-derived strain – that is, one which has evolved from a benign form of the virus which is used in vaccines to create immunity without causing illness. Though normally harmless, she said, the benign form can evolve back to a disease-causing form.
Anyone vaccinated will be completely protected from illness but can become contagious with the new, evolved virus that could threaten others. That is apparently what happened to the unvaccinated young man in New York.
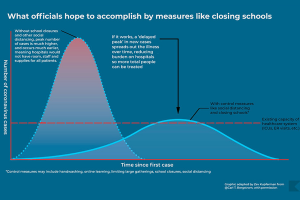
Dr. Higashi said that polio spread in Rockland County because of the high number of unvaccinated individuals.
“If you have a certain percentage of the population that isn’t vaccinated, there’s enough of the replication going through that virus that it can revert, it can mutate back to being a virulent strain that can cause paralysis,” Dr. Higashi said.
If the reverted strain spreads to Los Angeles, she said, any unvaccinated person could catch it and become ill.
“The most important thing is for us to look at the population who may not have been, you know, sort of on board with vaccination for polio and try to get those individuals vaccinated,” she said.
She said that some parts of the Jewish community are vaccine-resistant and recalled previous measles outbreaks which were focused in the Jewish area of Hancock Park.
At Shalhevet, Dr. Higashi said it would be difficult to get an exemption. She said students at California high schools must submit vaccination records when they enroll.
Personal belief exemptions were banned in a 2015 law signed by then-Gov. Jerry Brown. Now only medical exemptions, which must be signed off by a doctor, are permitted in the state.
Shalhevet Chief Operating Officer Ms. Sarah Emerson said Shalhevet follows that law.
“Shalhevet is in full compliance with California’s required vaccination schedule for students in public and private schools,” Ms. Emerson said in an email response to Boiling Point questions last month. “We will not be sharing any data regarding vaccination rates for particular immunizations.”
According to the CDC, monkeypox causes a rash that can occur on or near the genitals or anus but could also be on an infected person’s hand, face, chest, feet or mouth. Those who have the virus are able to spread it until the rash – which is typically very painful- is completely healed, usually around two to four weeks, meaning patients should isolate for that long.
The virus “can spread to anyone through close, personal, often skin-to-skin contact” and direct contact that can occur through intimate contact, the CDC said,
According to the County of Los Angeles Public Health, 2,231 cases of monkeypox had been confirmed in Los Angeles County as of Nov. 23, and two people have died.
Dr. Higashi encouraged vaccination and a heightened awareness for those in an affected community.
“The idea is that through education, access to the vaccines, the testing, the treatments, that we should be able to effectively limit the virus and eventually reduce the number of cases over time,” she said.
She added that although she doesn’t believe this is a disease that will spread in a school setting, schools should educate students on the risks.
“Just having folks understand the risk factors, and what their own personal risk is,” Dr. Higashi said.” My guess is that I don’t think that there’s zero risks – from the standpoint, it’s really important to know what the virus is, how it’s transmitted, who’s at risk, and what you can do to protect yourself if you’re at elevated risk.”
test2