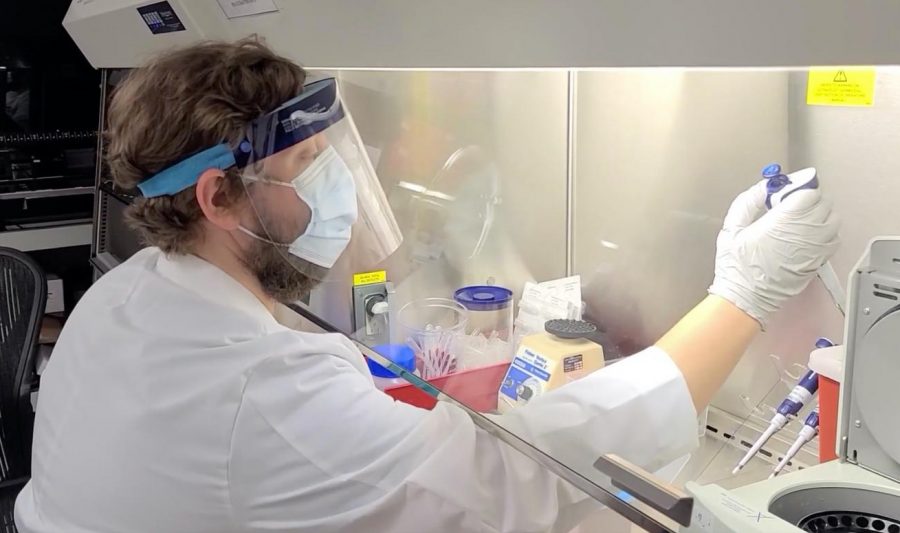
MASKED: Dr. Eric Vail works in the clinical molecular pathology lab at Cedars-Sinai, wearing PPE to protect himself from Covid-19 samples he is studying.
Just blocks from school, doctors searching for U.K. variant of Covid-19 discovered California’s
CAL-20C variant, identified at Cedars Jan. 3, is probably not resistant to vaccines, says doctor whose team found it
March 10, 2021
California is known for the beach, movie stars, fashion, and now for its very own coronavirus variant.
Originating in Southern California, this variant — called CAL.20C, or the California variant — has now spread to 19 other states, Washington D.C., and six other countries, including Israel. Scientists at Cedars-Sinai Medical Center believe the spread can be attributed to Californians traveling while infected.
The team at Cedars is led by Dr. Eric Vail and Dr. Jasmine Plummer, who along with Dr. Wenjuan Zhang were among the first to identify and study this variant back in December. While looking for signs of the United Kingdom variant in patients at Cedars.
Less than two miles up San Vicente Boulevard from Shalhevet and dressed in full PPEs, they prepare samples from hundreds of Cedars coronavirus patients for analysis by a machine called the NovaSeq 600 sequencer, which stands like a giant photocopying machine in their clinical molecular pathology lab.
“So it’s funny enough, we were looking for the UK variant the week between Christmas and New Year’s,” Dr. Vail told the Boiling Point. “We ended up loading the sequencer at 11 pm on New Year’s Eve, and we didn’t see the UK variant.”
However, on the morning of Jan. 3, something unexpected arrived in his inbox from Dr. Zhang, the lab’s bioinformatician, who would become the lead author of an article reporting the finding.

“[Dr. Zhang] emailed me on Sunday and said, ‘We’ve found something different here, that’s almost 40% of our samples from the end of December,’” Dr. Vail told the Boiling Point. “And then we got to work, and we mined the public databases to see if it was also there. And it was, and by the end of January it was 50% of all Covid cases from Southern California.”
Looking back through previous samples, Dr. Vail and his team were able to determine that the first case of the California variant was found in July, in Los Angeles County, reappearing in October and spreading rapidly in November and December. The surge in CAL.20C cases aligned with the holiday season — and also, the worst month for California so far in the Covid19 pandemic. On Dec. 29, cases in the county mushroomed to 21,648 in a single day.
It was the worst month of the pandemic in Southern California, so far.
Three weeks later, on Jan. 20 — as LA County deaths headed toward their one-day peak of 930 on Feb. 24 — Dr. Vail’s department published the first scientific journal article on the California variant, detailing the genetic mutations that differentiate this strain.
Dr. Vail is the assistant professor of Pathology and Director of Molecular Pathology in the Department of Pathology and Laboratory Medicine, and Dr. Plummer is a research scientist at the hospital’s Center for Bioinformatics and Functional Genomics; she is also Associate Director of the Applied Genomics, Computation & Translational Core.
Dr. Zhang works in the Department of Pathology and Laboratory Medicine at Cedars-Sinai.
Meanwhile, a team of scientists at University of California San Francisco, separately came across the California variant on New Year’s Eve. The two groups had similar results, and according to the New York Times, both found CAL.20C while looking for the UK variant, B.1.1.7.
According to Shalhevet Biology teacher Dr. Elizabeth Basheer, genetic mutations causing variants are mistakes that happen when a virus replicates. Dr. Basheer said this occurs in nature just as it does in human behavior.
“If I gave you a huge book and asked you to hand-copy it, you’re going to make some mistakes as you’re copying it,” Dr. Basheer said in an interview Feb. 25. “Same thing happens when the body copies DNA for a virus. There are chances that it gets copied wrong in some places. When it’s copied wrong, that’s a mutation.”
Dr. Vail and his colleagues found that CAL.20C is defined by five particular mutations to the Covid-19 virus. Two are located internally, inside the virus’s shell. These two mutations are less worrisome than the other three.
The other three mutations are located on the virus’s external “spike” proteins — the protrusions which give all coronaviruses their distinctive appearance, along with their name, corona, which is Latin for “crown.” These three are more concerning, because most vaccines now in use and being developed work by causing the body to make antibodies against the spike protein, which then make the virus incapable of entering human cells.
Mutations of the virus that change the spike protein’s shape can potentially make vaccines less effective, because the antibodies evoked by the vaccine won’t bind as well to it. Vaccines by Pfizer-BioNTech and Moderna, which are composed of “messenger RNA” — or mRNA — and Johnson & Johnson all target the spike protein, as do many other vaccines in use or in development around the world.
“The current mRNA vaccines are using the mRNA which codes for how to make that spike protein,” Dr. Basheer said. “The mRNA vaccine is then teaching our bodies how to recognize [and fight] the spike protein of the virus.”
The most notable mutation in the CAL.20C variant is a spike protein mutation called L452R, which is within a known receptor-binding domain (that is, an immunogenic piece from a virus that attaches to a specific internal receptor sequence to enter host cells) that has been found to be resistant to certain monoclonal antibody treatments against Covid-19, according to a journal article published about the L452R mutation back in July by the Elsevier Public Health Emergency Collection.
“There was a paper … that had looked at different mutations in the receptor binding domain and looked at their effect on monoclonal antibodies, and this one [ L452R mutation] was one of those that was resistant to one group of monoclonal antibodies,” Dr. Vail said.
Monoclonal antibodies can be used to treat Covid-19 in patients, “so it was definitely a mutation of interest for us from the very beginning,” said Dr. Vail.
How concerned was the Cedars team?
“I wouldn’t say concerned, I would say intrigued,” Dr. Vail said, describing his initial reaction to seeing the L452R mutation in the California variant.
But he said this does not mean the California variant will be resistant to the vaccine.
“I would say most likely not,” Dr. Vail said, even though at least one variant — the South Africa variant, also known as B.1.351 — has seemed to show reduced vaccine effectiveness.
“We think as a lab, and I think this is pretty standard in the scientific community, that most of these variants will not be resistant to the vaccines,” he said. “We’re definitely seeing huge reductions in mortality, huge reductions in severe disease from the vaccine, and I think that’s going to hold up regardless of the variants that emerge — possibly even the South African variant.”
Additionally, Dr. Vail said that there is a whole other branch of the immune system, the cellular immune system, that is “designed to kill intracellular organisms such as viruses and are targeted towards that and are very good at it.” In combination with the vaccine, this is an extra element protecting against new variants.
Because of this, he said, “it is very likely that even against these immune invasion strains we will still see very good benefit from the vaccines. Even if there is a small decrease in efficacy for symptomatic prevention, we expect at least a very high reduction in — almost a 100 percent reduction — in mortality and severe cases”
Still, Dr. Vail also shared that while it is not yet clear whether CAL.20C is deadlier than current Covid strains, “we’re pretty confident that it’s somewhat more infectious” and may be part of what drove the holiday spike.
Also, it is still unknown whether this variant typically is asymptomatic or symptomatic in those infected, but Dr. Vail thinks it will probably be more symptomatic.
To track the spread of CAL.20C, Dr. Vail’s lab is using an advanced technique called next-generation sequencing to analyze the virus’s genes in their clinical molecular pathology laboratory. This laboratory was originally used for analyzing genes related to oncology but shifted to a Covid-19 focus after the pandemic hit.
He said the virus samples being used for genetic sequencing were collected from patients at Cedars along with random samples of SARS-CoV-2 viruses in publicly available databases. The new samples collected are kept in –80 C° freezers while waiting to be sequenced.
After receiving a sample from an infected person, scientists put it in a test tube containing a solution called universal transport medium, which stabilizes the viral RNA. This solution is then processed, isolating the RNA.
Next, the researchers take this RNA and conduct “library preparation” where they break down the RNA into small fragments and attach a molecular barcode.
Then the RNA is enriched for the viral genome. In the RNA there is some RNA from the human host, which you don’t want to analyze, so you enrich it to get the part of the wanted RNA; this is called your library. In Dr. In Vail’s lab, this library is then loaded onto a sequencer with thousands of other samples, all uniquely barcoded, to receive sequencing results.
Those results are compared to a reference genome to see where in the RNA any mutations have occurred.

While interacting with these Covid samples in the lab, the scientists at Cedars wear full PPE including eye protection, double gloves, a back closing gown, and N95 masks. They also work in a negative pressure chamber.
“This is all done under very safe conditions to the point where not a single person has gotten infected from laboratory testing,” Vail said.
It takes a lot of time, and there’s much to be studied. Currently, Dr. Vail is working 60- to 70-hour weeks, including on weekends.
“We are now doing cell culture assays to look for increased growth in culture, [and] antibody neutralization assays,” he said. “We’re cloning the proteins with the specific mutations in them to look for decreased antibody sensitivity”
Looking at clinical data also reveals much about new strains to Vail and his team.
“We’re looking to partner with a couple different institutions to increase our sample size and get a lot more clinical data where we can get patient records to be able to look for these changes in morbidity, hospitalization, increased supplemental oxygen use, ventilation, things like that,” Dr. Vail told the Boiling Point. “And then we’re doing epidemiological studies as well.”
But even though Dr. Vail isn’t too worried about the California variant, he agrees with President Biden’s Covid Task Force that keeping the virus under control — and reducing it to as low levels as possible — is essential to prevent further spread of Covid-19.
That’s because every new case encourages the virus to keep mutating, scientists say, and mutations can be dangerous and compromise the effectiveness of certain Covid-19 treatments. So it is of paramount importance to prevent them from developing.
Dr. Anthony Fauci, President Biden’s Chief Medical Advisor, made that same point in a White House task force briefing Jan. 29, when urging people to get vaccinated as soon as they can.
“There is a fact that permeates virology, and that is that viruses cannot mutate if they don’t replicate,” said Dr. Fauci, a leading authority on viruses for more than 40 years.
“And if you stop their replication by vaccinating widely and not giving the virus an open playing field to continue to respond to the pressures you put on it, you will not get mutations.”
Dr. Vail agreed, noting that vaccine companies’ efforts to create “booster shots” to fight variants will always be running behind schedule of new mutations.
“I think the most important thing is don’t wait for a booster shot,” Dr. Vail told the Boiling Point. “If you can get a vaccine, please get a vaccine. Pfizer is for 16 and older so some of your readers will have the opportunity to get that.
“Until we are completely out of this, please continue to socially distance and wear a mask. Wash your hands. Do all the things so we can get out of this together, because the light’s at the end of the tunnel we’re almost there.”